The Prenatal Screen that I Recommend for My Daughter—The Full Integrated Screen

Deciding which prenatal screen to use can be confusing. I have been evaluating prenatal screening tests at Warde Medical Laboratory for the past twenty years. So, when my daughter, at age 32, told me that she was going to have her first baby, I shared my advice with her about the test that would maximize the chance of detecting a significant abnormality and minimize the chance of having a false positive (also called “screen positive”). After mentioning the advice I gave my daughter to some of my colleagues, they suggested that, while a bit personal, it may be useful to other individuals.
I’ll start with the bottom line. I recommend the Full (in some laboratories called the Complete) Integrated Screen Test. It gives the highest detection rate with the lowest false positive rate. To my way of thinking, it protects the fetus (my future grandchild) more from needless invasive procedures than the other available tests. It also gives my daughter the assurance that she has achieved the highest detection rate for the most common chromosomal abnormalities (Down syndrome-trisomy 21, and Edwards syndrome-trisomy 18) and open spina bifida (neural tube defects not covered by skin). And while it requires samples from both the late part of the first trimester and the second trimester, the final results can be available as soon as the middle of week 15 of her pregnancy.
The following is a made up question and answer session between a daughter and her pathologist father about prenatal screening.
Why do I need to do any prenatal screening?
To give you more information about your pregnancy so you can minimize the chance that a needless procedure will harm the health of your future baby and let you know if there is a significant possibility of a chromosomal problem with the baby.
But, I know that some people decide not to continue a pregnancy if these tests suggest Down syndrome or other problems. I don’t think I would wish to do that. Why should I do this testing?
In some cases, conditions such as open neural tube defects or other problems can be suspected by a positive Full Integrated Screen. Some of these conditions might alter how your obstetrician recommends you choose to deliver your baby for the improved health of that baby. For instance, if the information from the screening test and subsequent confirmatory tests show an open neural tube defect, your obstetrician may offer a Caesarian section to minimize potential trauma that the baby may sustain if she were to pass through the birth canal. Even if your baby has a genetic condition, by knowing about it ahead of time, you can begin to prepare for appropriate care. Lastly, while you currently believe that your decision is firm about continuing a pregnancy no matter what the finding, you may wish to keep an open mind to consider the information you are provided by the test and by the counseling given to you before and after the test by your health care provider.
Why is the Full Integrated Screen the test you recommend?
According to the information provided by the American College of Obstetrics and Gynecology (ACOG) in their January 2007 Practice Bulletin number 77, the Full Integrated Screen has the highest detection rate of the most common abnormalities with the lowest percentage of false positives. I prefer to use data from organizations such as ACOG, or large independent clinical studies involving multiple centers across the country such as that of Malone and coworkers published in the New England Journal of Medicine in November 2005. Some reference laboratories publish studies performed by their own employees, but to me, while they may provide useful information for the laboratory’s internal quality indices, there is an inherent conflict of interest in such work.
What is the Full Integrated Screen Test?
It requires a measurement of the space at the back of the neck called the Nuchal Fold Translucency (NT) by an ultrasonographer who has been specially trained and certified to perform this measurement. It also requires two blood samples from the mother.
The ultrasound that provides a precise estimate of the gestational age and the measurement of the NT is performed during the first trimester between weeks 10 and 13.
The first blood sample may be taken any time from week 10 through week 13 day 6 of the pregnancy. It is tested for PAPP-A (Pregnancy Associated Plasma Protein-A).
The second blood sample may be drawn anytime from week 15 until week 22, day 6. It is tested for AFP (alpha fetoprotein), uE3 (unconjugated estriol), hCG (human chorionic gonadotropin) and inhA (Inhibin-A). The earlier it is drawn, the earlier the final interpretation of the Full Integrated screen will be available.
After the second blood sample is received, the data from the first sample, the ultrasound measurement of the NT, and the data from the second sample are evaluated together with your personal information such as age, weight and family history to provide you with your risks for having a pregnancy that is affected by Down syndrome (trisomy 21), Edward syndrome (trisomy 18), open neural tube defect, and other less common problems.
When do I get my test results?
They should be available two to three working days after your second blood sample. They are reported as Screen Negative or Screen Positive.
But one of my friends got a first trimester test and that result was available by week 13 for her. Aren’t there tests that can be completed earlier?
Yes, and because some obstetricians recommend it, we offer it for individuals who wish this information. But I wouldn’t recommend it to my daughter, because the First Trimester Test gives more false positives compared to the Full Integrated Screen-and I consider each false positive a potential risk to the future baby. Further, since AFP testing cannot be performed until the second trimester, the first trimester test is not able to detect cases of open neural tube defects at all. Those wishing to learn of this will still need to wait until the second trimester for that information.
For the first Trimester Screening Test the ultrasound that provides a precise estimate of the gestational age and the measurement of the NT is performed during the first trimester between weeks 10 and 13.
The blood sample may be taken anytime from week 10 through week 13 day 6 of the pregnancy. It is tested for PAPP-A (Pregnancy Associated Plasma Protein-A) and hCG (human chorionic gonadotropin).
The First Trimester Screening test has various names from some commercial labs. While this is an excellent test to detect cases of Down syndrome a few weeks earlier, it gives about five times as many false positives for the same level of detection as the Full Integrated Screen.
How do you know that?
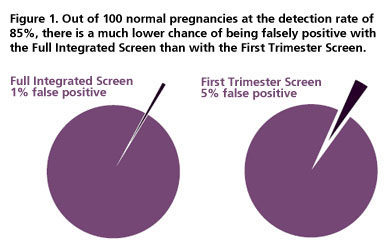
As I mentioned earlier, I believe the best information comes from independent data from many laboratories across the country, such as the large study reported by Malone et al. in the New England Journal of Medicine. According to that paper, the Full Integrated Screen can detect approximately 85% of cases of Down syndrome with only a 1% false positive rate, but to detect that many cases of Down syndrome, the First Trimester test gives 5% false positive results. To put these numbers another way, with the First Trimester Screening test about one out of every twenty women carrying a normal fetus will be told they are at increased risk for having a Down syndrome fetus. This compares with only about one out of one-hundred who would have this disturbing news if they use the Full Integrated Screen (figure 1).
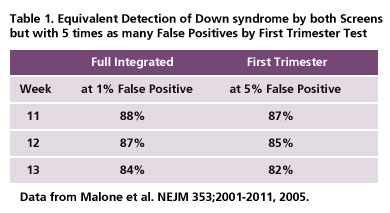
In Table 1, I show you some of the information from their study that compares the results of the First Trimester Screen with the Full Integrated Screen. It separates the information for samples taken during the first trimester at weeks 11, 12 and 13.
What’s wrong with getting a few more false positives with the First Trimester Screen?
A screen positive report, even though it is likely to be proven to be a false positive, is very disturbing information for you and your family. But most importantly it can increase the serious, potentially fatal consequences for the fetus (my grandchild in this case). About half the time, the mother who receives a screen positive report will choose to have an invasive procedure, a chorionic villus sampling (CVS) during the first trimester or an amniocentesis during the second trimester. These procedures are a significant risk to the life of the fetus. About 1 in 300 fetuses die following an amniocentesis and at least that number die following the first trimester procedure called chorionic villus sampling (CVS). Therefore, each false positive poses a risk to the fetus. Since my daughter’s concern was to have a live, healthy baby, minimizing the need for an invasive procedure (CVS or amniocentesis) is very important.
Don’t some laboratories claim a smaller false positive rate for their first trimester testing?
Yes, some have such claims. But when I review them with my own daughter in mind, I can’t help but note that they are not substantiated by independent studies from large national groups. I recommend you use information from ACOG and articles that to me seem to have less obvious conflict of interest, such as the Malone article (cited above).
But doesn’t having the information sooner make it easier for the mother if she chooses to terminate an affected pregnancy?
While first trimester testing does provide information sooner, some women I have spoken with are under the misconception that the first trimester test provides information two or three months sooner that the Full Integrated Screen. Let’s look at what I mentioned before about the timing of the test. The First Trimester Test is performed during the last few weeks of the first trimester (usually weeks 11, 12 and 13), while the Full Integrated Screen uses testing from those same weeks and can be completed as soon as the middle of week 15. Yes, it is later. We do offer the First Trimester Test for obstetricians who request it for their patients. It is a relatively good test, but for the same detection rate, carries a significantly higher chance of a false positive. To decrease the chances of needing an invasive procedure by as much as five-fold, I believe an extra three or four weeks is well worth the wait.
This is why I advise my daughter to get the Full Integrated Screen to maximize her chance of detecting the most common genetic abnormalities, while minimizing the chance of undergoing an invasive procedure that may harm or kill a normal fetus.
What if doctors in my area can’t provide the ultrasound testing to measure the nuchal fold? Should I just do second trimester testing, the QUAD test?
Not if your pregnancy is known during its first trimester. You can still use the Serum Integrated Screen. Like the Full Integrated Screen, this test measures PAPP-A on a serum sample taken from the mother at weeks 11-13. As soon as week 15 begins, the QUAD test may be performed and the combined information, just as with the Full Integrated Screen. In the practice bulletin, ACOG noted that at a 5% false positive rate, the Serum Integrated Screen detects 85-88% of Down syndrome cases while the QUAD test at a 5% false positive rate will detect 81%.
But, even 85 or 90% doesn’t sound that good. Why can’t I know for sure, 100%?
None of the screening tests currently available can detect all cases of Down syndrome or the other common abnormalities. The reason screening tests are used is that they pose no serious health risk to the mother or her fetus.
Right now, the only way to have 100% certainty is to perform an invasive test (either CVS or amniocentesis) on every pregnancy. This would result in a significant risk to the fetus you are carrying. Since my daughter’s concern was to have this baby, she needed to decide if she wished to risk its life to achieve this level of certainty. And that brings me back to why I recommend that she have the Full Integrated Screen. It gives the highest level of detection for the lowest false positive rate.
What test do you recommend for someone in her second trimester?
I recommend the QUAD test. It is exactly the same as the second sample for the Full Integrated Screen (AFP, uE3, hCG and inh-A) and is performed between week 15, day 1 and week 22, day 6. This is my test of choice if the pregnancy is advanced beyond the first trimester dates for testing at the time the patient sees her obstetrician.
An older test, the Triple test, does not include Inhibin-A. Because of that, it is more likely to give a false positive, and by now you know how I feel about them, and is also less likely to detect cases of Down Syndrome.
The QUAD test is readily available from high quality clinical laboratories. According to independent data reported by the American College of Obstetrics and Gynecology, if we used 5% false positive rate for both tests, the QUAD test would detect 81% of Down syndrome cases while the old Triple test would detect only 69%.
Summary
In conclusion, for all the daughters out there, I recommend the test that currently gives the best detection along with the fewest false positives. If you are in your first trimester, that is the Full Integrated Screen. If NT measurements are not available in your area, you can still get the Serum Integrated Screen. If you are in your second trimester, the QUAD test is preferred over the old Triple test.
For the vast majority of women who take the Full Integrated Screen the result is improved assurance with a significant decrease in invasive tests that threaten the baby. My daughter and I were happy with her result (Figure 2).

Figure 2.
Fewer false positives
means more healthy babies.
References
-
- American College of Obstetrics and Gynecology Practice Bulletin Number 77, Obstetrics and Gynecology 109;217-227, 2007.
-
- Malone, F. et al. First-trimester or secondtrimester screening, or both, for Down’s syndrome. First and Second-Trimester Evaluation of Risk (FASTER) Research Consortium. New England Journal of Medicine 353;2001-2011, 2005.
- Canick, J.A. et al. Comparison of serum markers in first-trimester Down Syndrome Screening. Obstetrics and and Gynecology 108;1192-1199, 2006.

