Editorial: Utilization and Interpretation of Epstein Barr Virus Serologies
We receive fairly frequent calls regarding the interpretation of Epstein Barr virus (EBV) antibody panels. Although we provide interpretive guidance with each panel result, the potential number of exceptions to typical result combinations may be daunting to the medical professional tasked with using these results to plan clinical management.[1] In many (or most) cases of suspected acute EBV infection, a formal EBV serology panel is not necessary for clinical diagnosis.[2] Following is a brief and practical review of the appropriate use and interpretation of EBV – associated laboratory testing.
Initial Workup of Acute Infectious Mononucleosis
The most common EBV-associated illness is acute infectious mononucleosis (IM) – a self-limited febrile illness most often encountered in adolescents and young adults. In most cases, a full battery of EBV serology is not necessary to make the diagnosis of EBV-associated IM, and the application of a simple clinicopathologic algorithm with eliminate the potential pitfalls inherent in interpreting the battery of antibodies assessed in a full EBV serology panel.
If a patient presents with clinical signs and symptoms typical of acute IM (for instance, an adolescent or young adult with fever, malaise, pharyngitis, enlarged tonsils, and cervical lymphadenopathy), then a complete blood count (CBC) with a microscopic examination of lymphocyte morphology should be performed. The peripheral blood findings of absolute lymphocytosis (absolute lymphocyte count in excess of 4 x 109/L in adolescents or adults) — or a relative lymphocytosis in excess of 50% of total leukocytes – combined with at least 10% of lymphocytes showing reactive features (Figure 1) and marked heterogeneity of lymphocyte morphology classify the patient as having an IM-like syndrome. From here, a heterophile screen (“Monospot”) may be performed. The heterophile screen (an assessment of antibodies directed against EBV but that react with certain non-viral substrates) is a quick option, often available as an in-office test. If the presenting signs and symptoms and peripheral blood morphology support an IM diagnosis, and if the heterophile screen is positive, then the patient should be diagnosed with EBV-associated acute IM, and a formal panel of EBV serologies is unnecessary. If the initial heterophile screen is negative, but remaining features support EBV acute IM, then the heterophile screen should be repeated in one to two weeks, since it may take some time for the heterophile antibody to develop in acute EBV infection.
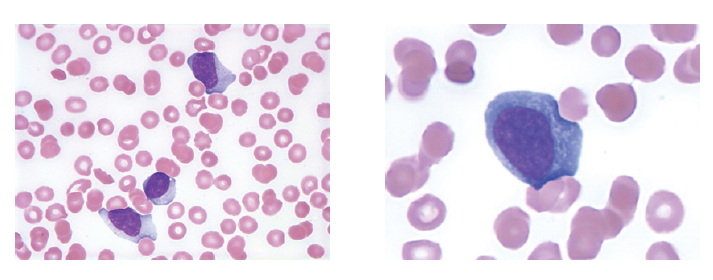
Figure 1. Reactive lymphocyte morphology in a patient with acute infectious mononucleosis caused by EBV. The presence of >50% lymphocytes on differential count, marked morphologic lymphocyte heterogeneity, and greater than 10% reactive lymphocytes in a peripheral blood smear, combined with typical clinical signs and symptoms and a positive heterophile screen, are typically sufficient to diagnose EBV-associated infectious mononucleosis.
The above approach will appropriately diagnose over 95% of adolescents or young adults who have EBV-associated acute IM.[2] However, a small minority of EBV-IM patients will not develop heterophile antibodies, or may present with an atypical clinical picture, and additional serologies detecting antibodies to specific EBV antigens may then be necessary.
Heterophile-Negative Infectious Mononucleosis
For those patients who do not develop heterophile antibodies in the setting of an IM-like syndrome, most will still have EBV-associated disease, and the diagnosis may be aided by assessment of antibodies to a series of EBV-associated antigens (Table 1). The panel generally used to assess for EBV infection includes antibodies to the viral capsid antigen (VCA) (both IgM and IgG), as well as IgG antibodies to early antigen (EA), and Epstein Barr nuclear antigen (EBNA).[1] Typically, VCA levels (IgM, with or without IgG) rise quickly in the first week or two of the acute infection, followed closely by a rise in EA IgG. VCA IgM will then generally subside within a month or two, while VCA IgG generally remains elevated for life in immunocompetent individuals. The duration of EA IgG antibodies is variable. In many individuals EA IgG subsides within six months to a year, but EA IgG may remain persistently elevated in a subset of individuals, potentially complicating the interpretation of serologic results. EBNA IgG is a late-onset antibody, generally appearing at about the time VCA IgM antibodies are subsiding, and usually indicates that the disease is progressing past the acute phase, or acts as evidence of past infection.
| No Past Infection | Acute Infection | Recent Infection | Past Infection | |
| IgM Anti-Viral Capsid Antigen (IgM-VCA) | – | + | +/- | – |
| IgG Anti-Viral Capsid Antigen(IgG-VCA) | – | +/- | + | + |
| Anti-Early Antigen (EA) | – | –/+ | + | – |
| Anti-EBV Nuclear Antigen (EBNA) | – | – | +/- | + |
Table 1. Typical serology patterns for antibodies against certain components of Epstein Barr Virus (EBV). Note that different variations of these patterns may exist. For example, some individuals harbor antibodies to EBV early antigen (EA) for a sustained period of time after acute infection, or re-acquire EA antibodies during reactivation infection. In many or most cases, a formal EBV serology panel is not necessary to diagnose acute infectious mononucleosis in patients with typical clinical features, typical blood smear morphology, and positive heterophile screen (see text above).
In a very small percentage of patients with IM-like symptoms, no evidence of EBV is found. In these patients, non-EBV-associated IM may be considered. Potential causes for IM-like symptoms in EBV-negative individuals are summarized in Table 2.[2]
| Infectious agents other than EBV |
| Cytomegalovirus |
| Acute HIV infection (at time of seroconversion) |
| Toxoplasma gondii |
| Human Herpesvirus-6 (Roseola) |
| Adenovirus |
Table 2. Infectious agents other than EBV that may cause infectious
mononucleosis-like syndromes. [2]M
Summary
In summary, the diagnosis of acute EBV-associated IM in most cases does not require an EBV serology panel, and potential confusion over the interpretation of a formal EBV panel therefore may be avoided. The appropriate age, appropriate clinical signs and symptoms, appropriate peripheral blood morphology, and a positive heterophile antibody screen are fully sufficient to render a diagnosis. However, a more extended serologic workup for EBV-associated antibodies may be indicated for patients who present with an incomplete set of diagnostic criteria, who present with atypical clinical features, for whom reactivation infection is suspected, or for whom assessment of previous EBV exposure status may be helpful clinically.
References
- Klutts JS, Ford BA, Perez NR, Gronowski AM: Evidence-based approach for interpretation of Epstein-Barr virus serological patterns. J Clin Microbiol 2009; 47(10):3204-3210.
- Peterson LC: Infectious mononucleosis and other reactive disorders of lymphocytes. In: Practical Diagnosis of Hematologic Disorders (5thedition). Kjeldsberg CR and Perkins SL, eds. Chicago: ASCP Press 2009:257-270.

