Ethyl Glucuronide: A Sensitive Marker for Alcohol Consumption

Background
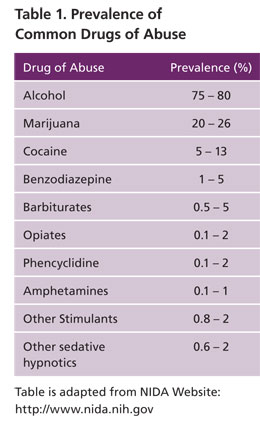 Alcohol (ethanol) is the most abused drug worldwide (Table 1). Alcohol abuse affects over 18.5 million adults in the U.S., costing society over $200 billion annually in lost productivity, health care expenditures, motor vehicle accidents, crime and other related costs 1. Alcohol related diseases contribute to a high percentage of all hospital admissions (more than 20 per cent) and deaths approximate 100,000 annually. Estimates also suggest that among children under age 18, one in four is exposed to family alcohol problems. Due to the host of medical, social, economic and personal afflictions associated with habitual drinking, it is essential that effective strategies be developed to prevent, diagnose, and treat alcohol-induced diseases as well as offenses 2. The development of effective diagnostic tests to detect high-risk drinking behavior and alcohol-induced tissue damage is therefore required for these strategies.
Alcohol (ethanol) is the most abused drug worldwide (Table 1). Alcohol abuse affects over 18.5 million adults in the U.S., costing society over $200 billion annually in lost productivity, health care expenditures, motor vehicle accidents, crime and other related costs 1. Alcohol related diseases contribute to a high percentage of all hospital admissions (more than 20 per cent) and deaths approximate 100,000 annually. Estimates also suggest that among children under age 18, one in four is exposed to family alcohol problems. Due to the host of medical, social, economic and personal afflictions associated with habitual drinking, it is essential that effective strategies be developed to prevent, diagnose, and treat alcohol-induced diseases as well as offenses 2. The development of effective diagnostic tests to detect high-risk drinking behavior and alcohol-induced tissue damage is therefore required for these strategies.
Metabolism of Ethanol
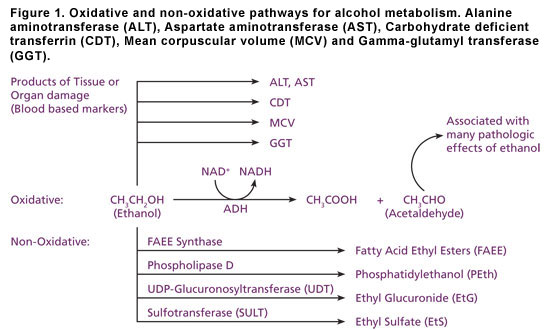
20% of ingested ethanol is absorbed in the stomach and another 80% in the intestine. This is distributed into the total body water representing 75% and 66% for men and women respectively. About 90% to 95% of ingested ethanol is oxidized in the liver by alcohol dehydrogenase, aldehyde dehydrogenase and microsomal ethanol-oxidizing enzymes before elimination in urine 3, 4.
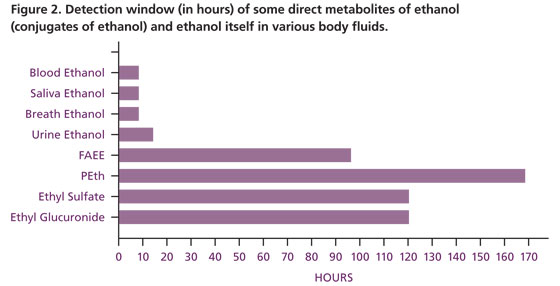
Some of these oxidation products are responsible for pathologic effects (Figure 1) often observed in individuals exposed to alcohol. Of the remaining ethanol less than 5% is eliminated unchanged in urine, sweat and breath. In these matrices ethanol itself must be measured in a relatively short time (less than 12 hours) post consumption in order for it to be detected (Figure 2). However, the non-oxidative products of liver ethanol metabolism (Figure 1) can be detected several days after ethanol itself has been eliminated.
Sensitivity and Specificity of Alcohol Biomarkers
Identification of any biomarker depends on how sensitive the detection method is for the analyte. High sensitivity (ability to correctly identify all individuals who have consumed alcohol) and specificity (ability to correctly identify all individuals who have not consumed alcohol) are essential qualities of a good marker. Traditional biomarkers for detecting chronic alcoholism tend to have moderate to high sensitivities and specificities. Unfortunately, some biomarkers for the detection of acute(recent) alcohol consumption such as ethanol itself, have high sensitivities but poor specificities (Table 2, Table 3) and a very short window of detection particularly alcohol itself (Figure 2).
Biomarkers of Alcohol Consumption
Indirect, oxidative biomarkers for detecting alcohol use, abuse as well as dependence in various settings such as work places and hospitals have been in clinical use for many years. However, the sensitivity and specificity of the methods used for many of these blood based biomarkers remain suboptimal. The emergence of non-oxidative direct metabolites of ethanol biochemical markers 5, 6 for the detection of alcohol consumption has grown in recent years. Biomarkers of alcohol consumption as a whole can be classified into the following three groups:
- Traditional or chronic biomarkers (Table 2)
- Acute biomarkers for recent alcohol consumption (Table 3)
- Trait (genetic) biomarkers
Traditional or indirect biomarkers are related to chronic alcohol consumption; they are associated with long-term exposure to high amounts of alcohol (more than 1000 g in 2 weeks) the consequence of which is organ or tissue damage. Such organ damages cause the release of enzymes such as gamma-glutamyl transferase (GGT), aspartate aminotransferase (AST) and alanine aminotransferase (ALT) into the blood or other body fluids. Other biomarkers of alcohol-induced tissue injury include alpha-smooth muscle actin (SMA), fibronectin, collagen type I, serum hyaluronate, matrix metalloproteinase (MMP)-2, and MMP-9. Biomarkers of prolonged fetal alcohol exposure and pancreatitis include fatty acid ethyl esters (FAEE), ethyl oleate, ethyl linoleate and carbohydrate-deficient transferrin (CDT) as shown in (Table 2).
Table 2. Traditional (chronic) biomarkers of ethanol consumption
| Marker | Sensitivity/ Specificity (%) | Potential or Current Use | Potential Source of False Positives | General Comments |
| Gamma-glutamyl transferase (GGT) | 61/ NA | Chronic alcohol abuse | Non-alcohol related conditions e.g. liver and biliary disease. Medications inducing microsomal enzymes. | Elevations are usually seen prior to the onset of pathologic consequences. Many sources of false positives. Characterized by about 70 drinks/wk for up to 2wk.. |
| Alanine Aminotransferase (ALT); Aspartate Aminotransferase (AST) | Method dependent 56 /NA | Chronic alcohol abuse. Not reflective of recent drinking. | Non-alcohol related conditions e.g. liver and biliary disease. Medications inducing microsomal enzymes. | Less useful for men than women. Reflective of some liver dysfunction. AST/ALT> 2.0 specific for ethanol-related liver diseases. |
| Carbohydrate deficient transferrin (CDT) | 83/92 | Heavy alcohol use. A good indicator of relapse | In iron deficiency, syndrome of carbohydrate deficient glycoprotein and fulminant hepatitis C. Inborn errors of glycogen metabolism. | Altered form of iron transport protein when drinking is continued for 2 or more weeks. Characterized by >60g/day for > 2 wks. |
| Whole blood associated acetaldehyde (WBAA)* | >95/95 | Abstinence, recent alcohol consumption. | N/A | Binds to proteins e.g. hemoglobin over a long period (120 days). |
| Mean corpuscular volume (MCV) | 47/ Moderate | Poor for relapse. Useful for heavy alcohol use. | Hemolysis, anemia, liver disease, Vitamin B12 deficiency | MCV increase with excessive ethanol intake (affects erythroblast development).Characterized by >60g/day for > 2 wks Slow return to normal limits even with abstinence. |
| Salsolinol | NA /NA | Promising for chronic alcohol consumption for babies of pregnant women. | N/A | More useful when measured in blood, but decreased in urine following acute drinking. |
| Acetaldehyde adducts | 70/93 | Hemoglobin-bound acetaldehyde adduct (HA) distinguishes heavy drinkers from abstainers | Diabetics tend to have twice the level of HA than alcoholics. Non-physiological administration of acetaldehyde | This is the first metabolite of alcohol consumption. There is a possible difference in sensitivity between men and women. Testing methodology is currently complex for routine testing. |
| Phosphatidyl Ethanol (PEth) | 92/100 | Chronic heavy drinking. Identifies relapse | PEth formation from blood containing ethanol during storage. | Formed in cell membranes only in the presence of ethanol. Characterized by ethanol >300 g for 1week. |
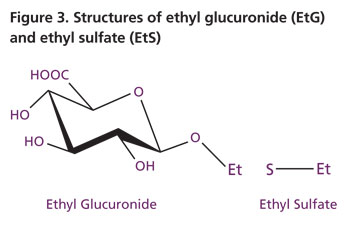
Acute or direct biomarkers (relapse markers) are sensitive enough to reflect a single recent intake of alcohol 7, 8. They include analytes such as ethyl glucuronide (EtG), ethyl sulfate (EtS), 5-hydroxytryptophol (5-HTOL) and ethanol itself. EtG and EtS are both conjugated direct metabolites of recent ethanol consumption. de Wildt et al. showed that the enzyme UDP-glucuronosyltransferase (UGT) catalyzes the reaction between ethanol and uridine-5-diphospho-β-glucuronic acid 9 to form EtG (Figure 1) whilst EtS is formed by conjugation with a sulfate involving a cytosolic sulfotransferase 10. Yet another acute marker of interest is fatty acid ethyl ester (FAEE), a product of fatty acids and ethanol catalyzed by the enzyme FAEE synthase.
Table 3. Acute (recent) biomarkers of alcohol consumption and emerging biomarkers
| Marker | Sensitivity/ Specificity (%) | Potential or Current Use | Potential Source of False Positives | General Comments |
| 5-hydroxytryptophol/5-Hydroxyindole-3-acetic acid 5-HTOL/5-HIAA | NA/ NA | Monitoring recent consumption of low levels of alcohol (sobriety) | Diet (bananas, pineapples). Drugs (disulfiram, cyanamide) | A serotonin metabolite measured in urine. |
| Fatty acid ethyl esters (FAEE) | 100/90 | Distinguishes heavy or alcohol dependents from social drinkers. | N/A | Present in fatty tissues, liver and pancreas up to 24 hrs after drinking. In hair for long periods. |
| Ethyl glucuronide (EtG), Ethyl sulfate (EtS) | >95/98 Cutoff=500ng/ml Warde Medical Laboratory | Forensic, monitors relapse | Unintentional exposure from OTC medications or personal hygiene items. | No gender, age or ethnicity effects known. Measured in urine, serum/plasma, tissues or hair |
| Sialic acid (SA) | 58/96 (women) 48/81 (men) | Monitoring heavy drinking. | SA increases in tumor patients, diabetes and in cardiovascular diseases. SA levels decrease after tumor treatment. | Non-alcoholics have less SA than alcoholics. Takes longer to decrease during abstinence. Measured in serum/plasma. |
| Ethanol | 88/92 for drinking > 50g/day | Monitoring recent or excessive consumption. | Bacterial fermentation of sugars in sample. | Rapid elimination (5 -8 hrs), thus, test is of limited use beyond this period. |
| Hexosaminidase | 94/91 | Heavy alcohol consumption. Detects drinking of more than 60 g/day for > 10 days. | Renal malfunction as in urinary tract malfunction, hypertension, diabetes and pregnancy. | Hexosaminidase concentrations are high in the kidney. Returns to normal levels pretty fast (up to 10 days of abstinence) |
Trait markers identify individuals with a genetic predisposition to alcohol consumption. These markers will usually be present irrespective of disease status implying that it is heritable. Candidate markers in this category include enzymes such as platelet monoamine oxidase (MAO) 11 adenylyl cyclase (AC) 6 and neurotransmitters like gamma-aminobutyric acid (GABA) which act on receptors in brain cells. Ratsma et al. (2002) found that GABA levels in people are different and inherited 12. Non-alcoholic individuals are reported to have a higher GABA level than those who tend to be dependent on alcohol. Differences in the opioid product of the pituitary gland beta endorphin have also been found among children of alcoholics who have fewer opioid receptors than those of non-alcoholics 13. If these trait markers prove to be useful, vulnerable individuals will be able to seek early treatment or prevent alcoholism altogether.
High sensitivity and specificity biomarkers with a long detection window
The measurement of ethanol itself is the most objective method for quickly confirming its presence in an individual of interest. However, the low specificity and very short window of detection renders ethanol itself a less suitable marker (Figure 2). Ethanol has an additional disadvantage that it can be detected in the sugar containing body fluids of diabetics exposed to bacteria. The ideal marker should be sensitive and specific as well as have a long window of detection (Figure 2). The desire for such biochemical markers has prompted the recent surge in the study and testing of EtG and EtS which have been proposed to meet these requirements 8, 14.
Ethyl Glucuronide (EtG) and Ethyl Sulfate (EtS)
Why measure EtG and or EtS?
EtG is a non-oxidative, non-volatile, stable and minor direct metabolite of ethanol (Figure 1). The advantages of testing EtG over other known biomarkers of ethanol consumption include the following:
- EtG has an additional advantage of being present in hair as well as the usual body fluids (whole blood, serum/ plasma, cerebrospinal fluid and urine). It is also reported to be present in body tissues such as liver, fat and brain.
- It is detected in body fluids even when there is no alcohol left in the body indicating that ethanol has recently been consumed.
- Serum EtG peaks 2 – 3.5 hours later than ethanol and can be detected for up to 5 days after ethanol itself has been eliminated from the body (Figure 2). Recently, EtG was detected in a corpse of a known alcoholic exhumed 27 years after death 15.
- Very sensitive and specific (see Table 5).
- Ideal for zero tolerance as well as abstinence.
- EtG is detected in urine only when alcohol is consumed and metabolized by the liver. Unintentional ethanol present in urine of diabetics as a result of bacterial fermentation of sugars in vitro does not metabolize to EtG.
- EtS has all the advantages of EtG. Unlike EtG though EtS is stable in urine at room temperature with no extrarenal sulfate conjugation (false positive) or de-sulfation upon storage (false negative). False negative EtG has been reported to occur by bacterial degradation (E. coli, the most common bacteria in clinical laboratories) and by high levels of β-glucuronidase found in urinary tract infections, kidney disease and bladder cancer. Recent reports indicate that false positive EtG can occur from in vitro bacterial conjugation of glucuronide to ethanol. However, this in vitro reaction can be prevented by refrigerating, freezing or collecting urine samples in NaF containers 14, 15, 16, 17.
- Low levels of EtG or EtS can occur from dilute urine. Low levels of EtG or EtS as a result of drinking large volumes of fluids prior to voiding can be corrected by calculating the EtG or EtS /creatinine ratio (UEtG100).
- EtG testing can be designed to include the simultaneous measurement of EtS in the sample such that they complement each other thereby unequivocally confirming alcohol intake.
Detection Methodologies for EtG and EtS
Currently the accepted testing methodologies for the detection of EtG and EtS in serum/plasma or urine utilize the following:
- Immunoassays (EIA and ELISA)
- GC/MS
- LC/MS and LC/MS/MS
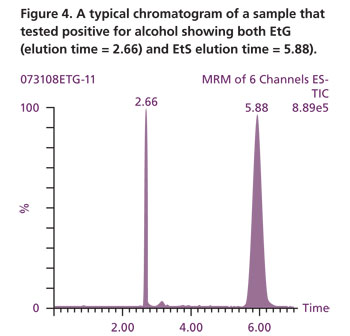 Warde Medical Laboratory employs enzyme immunoassays (EIA, supplied by Microgenics DRI® EtG) to screen urine samples for presumptive EtG positives at a cutoff of 500 ng/mL. All presumptive EtG positives (> 500 ng/mL) are confirmed using our state of the art LC/MS/MS technology. To unequivocally confirm ethanol consumption the Warde Medical Laboratory procedure for EtG testing has been optimized to simultaneously detect EtS as well in the same sample as shown in (Figure 4). Thus, a true positive for recent alcohol intake must have both EtG and EtS in the sample concurrently.
Warde Medical Laboratory employs enzyme immunoassays (EIA, supplied by Microgenics DRI® EtG) to screen urine samples for presumptive EtG positives at a cutoff of 500 ng/mL. All presumptive EtG positives (> 500 ng/mL) are confirmed using our state of the art LC/MS/MS technology. To unequivocally confirm ethanol consumption the Warde Medical Laboratory procedure for EtG testing has been optimized to simultaneously detect EtS as well in the same sample as shown in (Figure 4). Thus, a true positive for recent alcohol intake must have both EtG and EtS in the sample concurrently.
Cutoffs (decision levels) for Confirmed Positives
The principal concern for EtG or EtS testing is their very high sensitivity. EtG has been detected in samples of individuals who have used personal hygiene products such as mouthwash and many over the counter medications such as cough syrup and Nyquil (see Table 4 for a list of alcohol containing products). Eating alcohol containing foods, use of perfumes, aftershave, bug spray and antibacterial gels etc have all resulted in the detection of EtG in patient samples due to the very high sensitivity and specificity of the test.
Therefore there is the need to establish a dependable cutoff (level of alcohol) above which a test result is called positive and below which it is negative.
What is the cutoff of EtG or EtS?
At the present time, there is no consensus cutoff for EtG or EtS. Unintentional exposure to alcohol can result in detectable levels of EtG and EtS. The average person is exposed to more than one source of unintentional alcohol on a daily basis (see Table 4 for percentages of alcohol in items). Currently cutoffs of 100, 250, 500 and 1000 ng/mL have been used by different laboratories to confirm EtG. Concentrations between 25 -100 ng/mL have been used for confirming EtS.

At Warde Medical Laboratory, we are able to detect EtG down to 50 ng/mL (zero tolerance) and our evaluation of cutoffs at two different levels by LC-MSMS gave the following results:
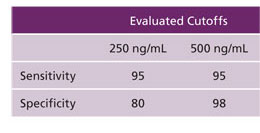
This is consistent with recent findings that levels of EtG greater than 500 ng/mL is associated with alcohol consumption 18. Additionally research has shown that incidental exposure will result in concentrations less than 500 ng/mL 19. In this study Costantino et al. (2006) showed that of 39 volunteers given a 4-oz bottle of mouthwash (12% ethanol) EtG levels in 12 were greater than 100 ng/mL, 3 tested greater than 250 ng/mL and one tested greater than 300 ng/mL. Individual programs may lower their cutoffs for EtG depending on their tolerance level for alcohol consumption.
Low cutoffs can detect relapses early but will also pick up unintentional exposure to alcohol. Setting high cutoffs will miss individuals with low alcohol levels in their system.
Consequently the US Department of Health and Human Services (US-DHHS) has issued an advisory regarding the use of this sensitive analyte 20.
EtG Advisory
The US-DHHS recognize that EtG and EtS are very sensitive and will detect unintentional exposure to alcohol (ethanol). The advisory therefore offered the following recommendations:
At low levels (in the region of the cutoff) of possible marker detection, EtG and EtS do not permit the distinction between alcohol exposure and alcohol consumption. As such evidence of disciplinary and legal action should not be based on the detection of EtG and or EtS alone. The advisory recommends that decisions be based on a combination of markers (see Table 2 and Table 3). The clinical condition and other information of the individual suspected of drinking should be evaluated as well as increasing the frequency of testing.
MROs investigating positive results are advised to be aware of a tests sensitivity, positive predictive value and potential sources of false positives.
Individuals targeted for testing should be advised to stay off items containing alcohol before alcohol testing.
Conclusion
EtG is a very sensitive biomarker of alcohol consumption. The concurrent presence of EtS in the sample adds value to EtG confirmation. However, like the initial concerns for the cutoff for the opiate morphine or Δ-9THC (cannabis), EtG lacks a universally established cutoff value at the present time. Until such a value is established, punitive measures against individuals with low EtG values alone is discouraged. It is advised to use a combination of alcohol biomarkers for such situations.
References
-
- Serdula M. K., Brewer R. D., Gillespie C., Denny C. H., and Mokdadm, A. Trends in alcohol use and binge drinking, 1985-1999., results of a multi-state survey. Am. J. Prev. Med., 2004; 26:294
-
- Meyerhoff D. J., Bode C., Nixon S. J., de Bruin E. A., Bode J. C., and Seitz H. K. Health risks of chronic moderate and heavy alcohol consumption: how much is too much? Alcohol Clin. Exp. Res., 2005; 29: 1334.
-
- Janda I. and Alt A. Improvement of ethyl glucuronide determination in human urine and serum samples by solid-phase extraction. J. Chromatogr B Biomed Sci Appl. 2001; 758 (2): 229-234.
-
- Jones A.W.. Urine as a biological specimen for forensic for forensic analysis of alcohol and variability in the urine-to-blood relationship. Toxicol Rev. 2006; 25(1):15-35.
-
- Sullivan J. L., Baenziger J. C., Wagner D. L., Rauscher, F .P., Nurnberger J. I. Jr., Holmes J. S. MAO in subtypes of alcoholism. Biological Psychiatry 2006; 27:911-922.
-
- Hellevuo K., Welborn R., Menninger J. A., Tabakoff B. Human adenylyl cyclase type 7 contains polymorphic repeats in the 3’ untranslated region: investigations of association with alcoholism. American Journal of Medical Genetics. 1997; 74: 95-8.
-
- Stephanson N., Dahl H., Helander A., Beck O. Direct quantification of Ethyl Glucuronide in Clinical Urine Samples by LC-MSMS. 2002; 24: 645-651
-
- Wurst F.M., Skipper G.E., and Weinmann W. Ethyl glucuronide – the direct ethanol metabolite on the threshold from science to routine use. Addiction. (suppl 2) 2003; 98 :51-61.
-
- de Wildt S.N.., Kearns G..L., Leeder J. S., van den Anker J. N. Glucuronidation in humans Pharmacogenetic and developmental aspects. Clinical Pharmacokinetics. 1999; 36: 439-452.
-
- Bernstein J., Meneses P., Basilio C., Martinez B. Further characterization of the pulmonary ethanol metabolizing system. Research Communications in Chemical Pathology and Pharmacology. 1984; 46:121-136.
-
- Sullivan J.L., Baenziger J.C., Wagner D.L., Rauscher, F.P., Nurnberger J.I. Jr., Holmes J.S. Platelet MAO in subtypes of alcoholism. Biological Psychiatry. 1990; 27: 911-922.
-
- Ratsma, J.E; Van Der Stelt, O and Gunning W.B. Neurochemical markers of alcoholism vulnerability in humans. Alcohol and Alcoholism. 2002; 37 (6):522-533.
-
- Zalewska-Kaszubska, J. and Czarnecka, E. Deficit in beta-endorphin peptide and tendency to alcohol abuse. Peptides 2005; 26(4):701-705.
-
- Wurst F.M., Wiesbeck G.A., Metzger J.W., Weinmann W. On sensitivity, specificity, and the influence of various parameters on ethyl glucuronide levels in urine-results from the WHO/ISBRA study. Alcohol Clin Exp Res. 2004; 28:1220-1228.
-
- Politi L, Morini L, Mari F., Groppi A., Bertol E. Ethyl glucuronide and ethyl sulfate in autopsy samples 27 years after death. Int. J. Legal Med. 2008; 122 (6): 507-9.
-
- Helander A., Beck O. Mass spectrometric identification of ethyl sulfate as an ethanol metabolite in humans. Clinical Chemistry. 2004; 50: 936-937.
-
- Helander A., Beck O. Ethyl sulfate a metabolite of ethanol in humans and a potential biomarker of acute alcohol intake. J. Anal. Toxicology 2004; 29: 270-274.
-
- Bottcher M., Beck, O. and Helander, A. Evaluation of a new immunoassay for urinary ethyl glucuronide testing. Alcohol and alcoholism. 2007; 1-3.
-
- Costantino A., Digregorio E.J., Korn W., Spayd S., and Rieders F. The effect of the use of mouthwash on ethyl glucuronide concentration in urine. Journal of Analytical Toxicology. 2006; 30: 659-662.
- Substance Abuse Treatment Advisory, US Department of Health and Human Services, 2006 Vol. 5, Issue 4.

