Serologic Testing for Lyme Disease
 We frequently receive calls regarding recommendations for Lyme disease testing. Due to recent minor changes to our Lyme disease test menu, we are taking this opportunity to clarify recommended approaches for the serologic evaluation of patients suspected to have Lyme disease.
We frequently receive calls regarding recommendations for Lyme disease testing. Due to recent minor changes to our Lyme disease test menu, we are taking this opportunity to clarify recommended approaches for the serologic evaluation of patients suspected to have Lyme disease.
Lyme disease is the clinical syndrome caused by infection with the bacterial spirochete Borrelia burgdorferi. Infection by B. burgdorferi is transmitted via the North American deer tick (Ixodes sp). In its initial phase, Lyme disease typically is characterized by a distinct pattern of rash known as erythema migrans (EM). [1, 2]
The incubation period between initial exposure and onset of EM varies considerably, but typically is about one to two weeks. [3] In the acute phase of infection, the rash may be accompanied by systemic symptoms such as fever, joint and muscle pain, generalized weakness or fatigue, and enlarged lymph nodes. If left untreated, Lyme disease may progress beyond the initial localized cutaneous phase into disseminated phases of disease.
 The early disseminated phase of disease may be marked by multifocal EM type rashes that occur days or weeks after initial exposure. It also may be marked by neurologic symptoms such as facial nerve palsy (Bell’s palsy), arthritis, or meningitis. If untreated, over half of patients will progress to a late disseminated phase, often marked by intermittent bouts of severe arthritis. A small minority of untreated patients will develop chronic neurologic symptoms such as pain or tingling in the hands and feet, or a mild encephalopathy manifest as difficulty in concentration, or deficits in memory. [3]
The early disseminated phase of disease may be marked by multifocal EM type rashes that occur days or weeks after initial exposure. It also may be marked by neurologic symptoms such as facial nerve palsy (Bell’s palsy), arthritis, or meningitis. If untreated, over half of patients will progress to a late disseminated phase, often marked by intermittent bouts of severe arthritis. A small minority of untreated patients will develop chronic neurologic symptoms such as pain or tingling in the hands and feet, or a mild encephalopathy manifest as difficulty in concentration, or deficits in memory. [3]
About 10 to 20% of patients will continue to have symptoms after a full course of antibiotic therapy for Lyme disease, a pattern referred to as post-treatment Lyme disease syndrome. [2, 3] The cause of this syndrome is likely related to some combination of residual tissue damage and autoimmune phenomena, and not to continuing active infection. This is an important point, since continuing antibiotic therapy in patients with post-treatment Lyme disease syndrome is generally not indicated, and may actually be detrimental. [3] In a vast majority of patients, these symptoms eventually clear, but ultimate resolution may take weeks or months. [3]
| Initial Localized Phase | Early Dissemination Phase | Late Dissemination Phase | Post-Treatment Syndrome |
| • Localized infection • Solid red or distinctive bulls-eye rash • Flulike symptoms; muscle and joint pain, headache, fatigue • Regional lymphadenopathy | • Multiple rashes • Cranial nerve palsy • Meningitis • Joint and muscle pain, fever, headache, stiff neck, vision problems, sore throat, fatigue, lymphadenopathy • Rarely; heart complications | • Recurrent arthritis • Neurological disorders; confusion, dizziness, short-term memory loss, disorientation • Peripheral neuropathy; pain and tingling in hands and feet | • Continuation of symptoms after full course of antibiotics; arthritis, peripheral neuropathy, leukoencepahlitis, encephalopathy, fatigue |
Laboratory Evaluation of Suspected Lyme Disease
Before discussing recommended laboratory tests, it is important to note that Lyme disease serologic testing should only be performed on individuals for whom there is sufficient clinical suspicion for Lyme disease based on clinical history, physical examination findings, and presence in an area endemic for Lyme disease. [1, 3] As is the case with many clinical tests, wide-spread serologic screening in the absence of pre-test suspicion adversely affects the performance characteristics of the testing algorithm, and increases the incidence of false positive results. [4]
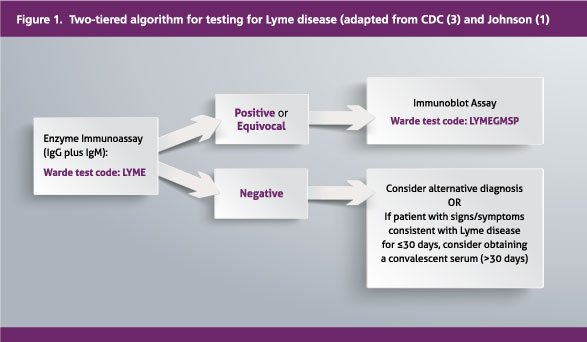
For patients with clinical signs, symptoms, and history suspicious for Lyme disease, the current standard is a two-tiered serologic approach, originally proposed at a multiagency consensus conference in 1995, and still endorsed by the Centers for Disease Control and Prevention (CDC) (Figure 1). [1, 3] The first tier involves enzyme immunoassay (ELISA)-based screening for both IgM and IgG antibodies against B. burgdorferi. At Warde Medical Laboratory, we offer a combined IgG / IgM (“total”) screen on the DiaSorin Liaison platform that targets the immunodominant Borrelia antigen V1SE (variable major protein-like sequence expressed) (Warde test code: LYME). [1,]
Previously, some laboratories were offering separate initial ELISA evaluations for IgM antibodies and for IgG antibodies, and this option was available through Warde. However, CDC recommends testing for both antibody types at initial evaluation, and there is no particular advantage in separating these analyses at initial diagnosis. Inclusion of IgM antibodies in the combined (total) serologic screen enhances sensitivity of the assay, since IgM may be present early in the course of infection relative to IgG. However, since both IgM and IgG antibodies may wax and wane, and since IgM antibodies may be present years or decades after initial infection, the mere presence of IgM antibodies does not necessarily indicate more recent infection, [1, 5] and reference laboratories are generally moving toward the combined (total) screen.
If the initial screen is either positive or equivocal, then the recommended second tier involves a supplemental analysis either by Western blot or similar immunoblot procedure (Warde test code: LYMEGMSP) (Figure 1). [1, 3] The inclusion of the second tier of evaluation for initial positives substantially improves diagnostic conditions (including other spirochete infections, and non-spirochete-associate disorders such as infectious mononucleosis). [6] Positivity for both the initial serologic screen and the subsequent immunoblot is considered evidence of infection (either past or current) by B. burgdorferi. The immunoblot step of the algorithm generally involves evaluation for IgG antibodies initially, and reflexes to detection of IgM antibodies if the IgG immunoblot is negative.
Direct methods of detection of B. burgdorferi (culture and DNA-based PCR analysis) are generally not recommended for initial screening for a diagnosis of Lyme disease.[1, 3] Culture methods are generally insensitive, especially in the disseminated phase of disease when interest in laboratory-based diagnosis is highest. While PCR testing may be useful in certain targeted settings (e.g. analysis of synovial fluid in suspected treatment-resistant Lyme arthritis), it is insensitive as an initial screening method. Also, PCR may detect DNA from non-viable organisms in patients successfully treated for Lyme disease, further complicating interpretation of a positive result. [3]
Limitations of Screening
Serologic testing for Lyme disease is sometimes criticized as being insensitive, but it is important to recognize the performance characteristics of these tests in appropriate clinical context. It is true that in the earliest phase of the disease, sensitivity is relatively low since antibodies take time to develop. That is why initial treatment for acute Lyme disease is often started empirically based on presentation with characteristic clinical findings (such as EM) in an area endemic for Lyme disease. [1] In general, the more time passes, the higher the sensitivity of the assay. According to Johnson. [1] while perhaps 60% of patients with EM will test positive with modern assays on initial Lyme serology, the detection rate for these assays climbs to nearly 100% in some studies after the EM phase of the disease, or after the first 30 days following initial infection. Similarly, specificity of the recommended two-tiered approach in patients at 30 days duration of disease or longer likely exceeds 95%. [7]
It is also important to follow the testing algorithm as written. While the use of immunoblot / Western blot methods enhances specificity, the use of immunoblots on patients who have not been initially screened using ELISA methods results in high false positive rates, and decreases in test specificity. This is particularly true for IgM-based blots, which rely on the demonstration of fewer individual bands for a positive tests than IgG-based Western blots, and which are generally more prone to cross-reactivity. [1]
Summary
Lyme disease testing should only be sought in patients for whom there is appropriate clinical suspicion for active Lyme disease (either acute or disseminated phase) based on clinical history, signs, and symptoms. Clinicians should use appropriate judgment for possible empiric treatment for patients who present with the classic erythema migrans rash in areas endemic for Lyme disease, as this phase of the disease may be difficult to confirm using laboratory methods.
For laboratory evaluation of Lyme disease, the CDC recommends a two-tier diagnostic approach. The first tier includes ELISA-based detection of IgM and IgG antibodies in a single combined assay (Warde test code LYME). A positive or equivocal ELISA screen should be followed up by an immunoblot-based method (Warde test code LYMEGMSP).
References
- Johnson BJB. Laboratory diagnostic testing for Borrelia burgdorferi infection.In: Halperin JJ, editor. Lyme Disease: An Evidence-Based Approach. Croydon, UK: CAB International; 2011. p. 73-88.
- Marques AR. Lyme disease: a review. Current allergy and asthma reports. 2010;10(1):13-20.
- Centers for Disease Control and Prevention. Lyme Disease. Available from: http://www.cdc.gov/lyme. Accessed 9/26/2014.
- Finn WG. Pre-test probability matters: a comment regarding "shotgun" testing. Warde Report. 2013;23(1):7.
- Kalish RA, McHugh G, Granquist J, Shea B, Ruthazer R, Steere AC. Persistence of immunoglobulin M or immunoglobulin G antibody responses to Borrelia burgdorferi 10-20 years after active Lyme disease. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2001;33(6):780-5.
- Bruckbauer HR, Preac-Mursic V, Fuchs R, Wilske B. Cross-reactive proteins of Borrelia burgdorferi. European journal of clinical microbiology & infectious diseases: official publication of the European Society of Clinical Microbiology. 1992;11(3):224-32.
- Molins CR, Sexton C, Young JW, Ashton LV, Pappert R, Beard CB, et al. Collection and characterization of samples for establishment of a serum repository for lyme disease diagnostic test development and evaluation. Journal of clinical microbiology. 2014;52(10):3755-62.

